March 26, 2019
Interoperability Battle Lines: Data Freedom Fighters vs. Entrenched Data Blockers

On a cold Minnesota morning in January 2018, Fairview Health Services CEO James Hereford addressed Twin Cities business executives regarding healthcare IT and innovation. (1) With an advanced degree in statistics and Silicon Valley “street cred” from his time as Stanford Health Care’s Chief Operating Officer, Hereford delivered a powerful critique of Epic Health System’s “walled garden” approach to managing healthcare data.
I will submit that one of the biggest impediments to innovation in health care is Epic, because the way that Epic thinks about their [intellectual property] and the IP of others that develop on that platform. There are literally billions of dollars in the Silicon Valley chasing innovation in health care. And yet Epic has architected an organization that has its belief that all good ideas are from Madison, Wisconsin. And on the off chance that one of us think of a good idea, it’s still owned by Madison, Wisconsin.
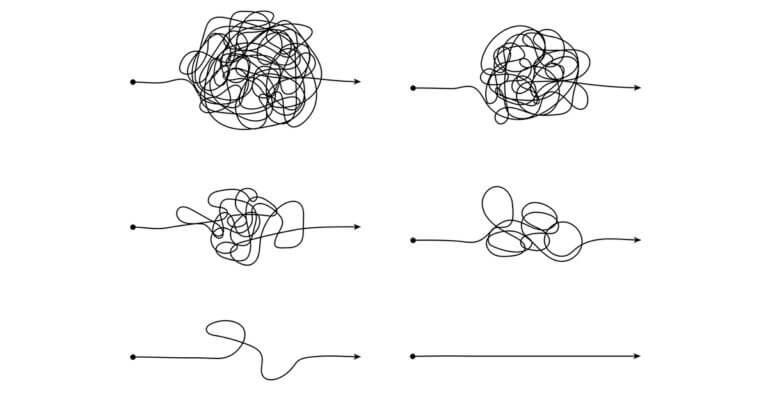
As illustrated by Hereford’s powerful rhetoric, a revolutionary battle is brewing over data interoperability and data blocking. Proposed regulations issued in February, 2019, by the Office of the National Coordinator of Health IT (ONC) and the Centers for Medicare and Medicaid Services (CMS) are at the forefront of a titanic struggle to liberate health data. If implemented with integrity, they will stimulate game-changing innovation that will save lives, minimize error, reduce caregiver stress, lower costs and enhance consumer experience.
However these new regulations threaten the monopolistic business practices of entrenched data oligarchs, most notably EHR vendors. Under the pretense of a shared commitment to data interoperability, they are organizing to diminish the impact of the proposed rules.
Together, the proposed ONC (771 pages) and CMS (251 pages) regulations are massive, detailed documents. The rules are well-crafted but, without vigilant defense, they are subject to manipulation. As currently drafted, the new regulations will take effect in 2020. Unless extended, the public comment period on the new rules will end in May 3rd, 2019.
Between now and adoption of the final regulations, data oligarchs and their minions will seek to water down provisions and penalties governing interoperability and data blocking. Data freedom fighters must blunt those attempts to maintain the unacceptable status quo. Let the battle begin.
THE UNFULFILLED PROMISE OF ELECTRONIC HEALTH RECORDS
In his 2004 State of the Union address, President George W. Bush sought to transform healthcare data management from 19th century paper records to 21st century digital records. The President created the ONC to “provide the national leadership and coordination” to achieve the following 10-year goals for electronic health records (EHRs).
- Electronic health records would ensure that complete health care information is available for most Americans at the time and place of care, no matter where data originates.
- These electronic health records would be designed to share information privately and securely among and between healthcare providers when authorized by the patient.
In President Bush’s vision, digitized EHRs would enable health companies to generate consistent high-quality outcomes, reduce performance variation and improve operational efficiency. Data inputs would flow freely and safely to improve care design and execution.
For patients, all relevant data from all sources would flow into algorithms that optimize diagnosis and treatment. As data proliferates and analytics advance, individualized genetic and environmental characteristics now lead to more personalized therapies; more precision and less trial-and-error care. At the disease level, all relevant information from all sources flows into data systems advancing medical research and protocol development.
The push toward digitized health records received a major boost in 2009 when Congress passed the HITECH (Health Information Technology for Economic and Clinical Health) Act. HITECH provided almost $40 billion in funding to digitize health records, accelerate EHR adoption and promote interoperability. The Act also introduced “meaningful use” standards to assess the use of EHR technologies “in ways that can be measured significantly in quality and in quantity.” (2)
HITECH’s massive investment accelerated EHR adoption. Today, 96% of hospitals and 86% of office-based physicians employ EHRs. Fewer than 10% of hospitals employed EHRs before 2008. (3)

In the process, the EHR ecosystem has grown from a disparate group of spirited, early-stage companies into a massive $13 billion industry. Two companies, Epic and Cerner, provide EHR services to over half of U.S. hospitals. (4)
In many respects, the nation’s investment in EHRs has backfired. A recent investigative report, “Death by a Thousand Clicks: Where Electronic Medical Records Went Wrong,” by Kaiser Health News and Fortune chronicles a litany of unintended consequences related to EHR adoption. These include upcoding, a flood of false alarms, physician burnout, medical errors, blocked data access, gag clauses and patient harm. Some of the report’s findings are truly alarming.
- Based on extensive interviews, KHN/Fortune conclude that EHR implementation has been “a tragic missed opportunity. Rather than an electronic ecosystem of information, the nation’s thousands of EHRs largely remain a sprawling, disconnected patchwork… that has handcuffed health providers to technology they mostly can’t stand.”
- 21% of people surveyed by Kaiser Family Foundation found mistakes in their EHR.
- Safety-related incidents related to EHRs and other IT systems are skyrocketing.
- An ER doctor makes roughly 4,000 computer clicks over the course of a single shift. This labor-intensive data-entry process invites error and causes physician burnout.
- Alarms, many of which are false, account for 85% to 99% of EHR and medical device alerts. Clinicians can’t tell which alerts contain the information they need to act.
Performance improvement’s first principle is to fix systems before automating them. With the government’s help, healthcare has automated a fragmented, error-prone delivery system riddled with perverse incentives.
Moreover, personalized clinical healthcare data may be humanity’s most difficult data set to manage. State-specific individual consent requirements for health data use further hamper accessibility. Collecting, curating and analyzing these data sets is a daunting challenge even with the most advanced technology platforms.
Recognizing the inherent complexities required to liberate healthcare data, the 21st Century Cures Act (passed in 2016) instructed the executive branch to develop regulations that “advance interoperability and support the access, exchange, and use of electronic health information; and address occurrences of information blocking.” The proposed ONC and CMS regulations respond to this legislative directive.
When President Bush announced ONC’s creation in 2004, annual U.S. healthcare expenditure totaled $1.6 trillion and annual estimates of preventable hospital deaths approached 100,000. In 2019, annual health expenditure is $3.7 trillion and preventable hospital deaths may exceed 400,000 per year. (5)
Perverse incentives encourage EHR vendors and users to block access to essential healthcare data. This has created an unhealthy codependence between EHR vendors and their provider clients.
DESTRUCTIVE CODEPENDENCE BETWEEN EHR VENDORS AND USERS
Consolidation within the EHR marketplace mirrors consolidation that is occurring among hospitals and doctors. Consolidation enables large EHR companies and large healthcare delivery companies to engage in anticompetitive behaviors. Reduced competition among hospitals, for example, leads to higher prices and suboptimal care outcomes. (6)
Large EHR companies and large healthcare companies coordinate to digitize and distribute health data. These coordinated efforts contribute to market dominance and pricing leverage. For example, closed EHR systems are lucrative for EHR vendors and enable health systems to reduce “leakage.” Health systems don’t want consumers to receive out-of-network care.

Advocates of hospital mergers often cite EHR consolidation as a merger benefit and necessity for improved care outcomes and cost reduction. A massive study published in Health Affairs examining hospital mergers between 2012 and 2016 found limited evidence of proactive EHR consolidation. Only a third of acquired hospitals switched EHRs. Moreover, those that switched increased Epic’s and Cerner’s market concentration.
As with so much in healthcare, EHR’s fundamental flaws originate in transactional, activity-based, fee-for-service payment methodologies. EHR’s principle function is to document treatment activity for billing, not advance clinical outcomes. Providers document treatment activity to optimize revenue generation through their billing and collection practices.
Much, perhaps most, of EHR’s administrative burden for providers relates to treatment documentation. As a consequence, providers can use EHR software to defraud payers by mispricing and overcharging for services delivered. Regulators term this practice “upcoding.”
However the insidious nature of EHR-health company relationships goes beyond perverse financial incentives. EHR companies often become essential components of their clients’ cultures and operations. From a position of deep trust, they deepen service offerings, stifle innovation and limit competition. The following factors contribute to this dystopian paradigm:
- Co-opted IT Departments: Hospital IT departments work in close concert with EHR vendors to implement massive installations. The EHR companies work very hard to create a “we’re in it together” mentality. For example, Epic sponsors memorable user conferences at its “Willy Wonka-like” campus in Verona, Wisconsin. (7) Excessive loyalty to their EHR vendors leads many EHR clients to accept inferior versions of vendor-sponsored applications, tolerate cumbersome workarounds and endure system underperformance.
- Enormous Switching Costs: In his article, “Why Doctors Hate Their Computers,” (8) Atul Gawande describes Epic’s exhaustive EHR training program at Partners HealthCare system. The majority of Partners’ staggering $1.6 billion EHR implementation cost went to tech support and patient revenues lost during training. Essentially, Partners is converting its operational practices to Epic’s standards, rather than Epic tailoring its software to Partner’s operating characteristics. Reeducation is time consuming, expansive and expensive. Like the pig debating a chicken regarding a ham and egg breakfast, Partners switching to the Epic EHR required “full commitment.”
- Nefarious Licensing Agreements: EHR vendors use their licensing agreements to solidify their control of source code and data. They consider their source data proprietary, even though it’s primarily patient data, and will not allow third parties to access it without their permission. Carefully worded legal agreements prevent health companies from commercializing innovative applications. Data sharing, to the extent it occurs, is one way — into, not out of, the EHR. Efforts to stimulate app development are equally one sided.
Accessing source data is an epic challenge for third-party app developers. Pun intended. No EHR vendor facilitates seamless access, but Epic is the most zealous in controlling and blocking its source data. In a 2002 interview, Epic founder and CEO Judy Faulkner described the company’s mission as “Do good, have fun and make money.” (9) It’s certainly worked for Faulkner. With a net worth of $3.5 billion, she is America’s third-richest self-made woman. (10)
Even with obstacles, solutions such as Infor’s Cloverleaf, Corepoint or InterSystems achieve data interoperability via published standards. Dozens of app developers use middleware companies, like MultiScale, Redox and Sansoro, to acquire targeted patient information and / or application development platforms like Apervita. Even these solutions must overcome cumbersome EHR data access and blocking.
Health data, like all data, must flow freely and easily to generate the greatest benefit. Limiting or blocking access to data is the major reason that EHRs have underperformed. Addressing the market failures embedded in current EHR practices requires pro-market regulatory intervention that makes healthcare data readily available to third parties.
ACHIEVING REGULATORY BALANCE
Regulation exists to keep people safe and to ensure level-field competition. Achieving balanced regulation is an art. Rules must be strong enough to restrain anticompetitive behaviors and flexible enough to avoid unnecessary burden. The proposed ONC and CMS regulations achieve this delicate regulatory balance.
ONC’s proposed regulations focus on interoperability while CMS’s proposed regulations focus on increasing patient access to their medical data. Together, they create a framework for the secure data sharing that will grants data access to patients and app developers.
In a recent blog post, Dr. David Levin describes this new framework as Health IT 2.0. Levin, the former Chief Medical Information Officer at the Cleveland Clinic, characterizes this breakthrough moment in healthcare technology as follows,
Health care is following the example set by the rest of the modern digital economy and starting to leverage existing monolithic applications like electronic health records to create platforms that support a robust application ecosystem. Think “App Store” for healthcare and you can see where we are headed.
Reinforcing Levin’s observation, ONC head Dr. Donald Rucker made the following observation in an interview accompanying the release of the proposed regulations,
…there is no Uber or Lyft in healthcare. There’s nothing really like a robust banking application or an aggregator site for healthcare. And there just hasn’t been really entrepreneurial activity in this space because people haven’t had any access to the data. And what data has been accessed is very, very guarded, very proprietary and I think we’re going see new business models here.
Key provisions of the proposed ONC regulations include the following:
- Pro-Competitive Provisions (page 206): The ONC rule supports business practices that “promote the efficient access, exchange and use of EHRs to support a competitive marketplace” that enhances value and choice. The commentary warns incumbent vendors they “must not interfere with a healthcare provider’s use of their acquired API technology in any way.”
- Broad Definition of Information Blocking (page 356): The information-blocking provisions in the proposed regulations are extremely broad. The commentary clarifies that information blocking comes in many forms, including “practices that limit the utility, efficacy, or value of EHI that is accessed, exchanged, or used, such as by diminishing the integrity, quality, completeness, or timeliness of the data.”
- Essential Interoperability Elements (Section VIII): In its discussion of data-blocking rules, the ONC addresses common challenges faced by digital health companies seeking to access data within EHR platforms. The commentary specifically warns vendors of certified health IT records systems, such as Epic and Cerner, to refrain from data-blocking behaviors.
THE EHR EMPIRE STRIKES BACK
The public comment period for the proposed regulations ends on May 3rd, 2019. In their own words, the Electronic Health Record Association represents “more than 30 companies that supply the vast majority of EHRs to physicians’ practices and hospitals across the United States.” On March 4th, 2019, the Association sent a letter to ONC head Dr. Rucker formally requesting “a 30-day extension of the comment period to June 3, 2019.”
The Association asserts it requires the additional time to survey their members to provide adequate feedback to ONC on the proposed regulations. The letter also questions whether the 24-month implementation period is sufficient. They warn of “unintended consequences” and “added provider burden” that could accompany the new rules.
What the Association is really doing, of course, is seeking more time to shape the new regulations. That’s what lobbyists do — tilt regulations to benefit their clients. When successful, pro-business interests overwhelm the pro-market interests of the American people.
As detailed in the KHN/Fortune report, EHR companies have demonstrated a callous disregard for patients and care providers. It is beyond time to implement regulatory adjustments that liberate health data and advance care delivery. It’s now time to realize the full promise of EHR technologies. They should make the lives of consumers and care providers both better and easier.
JUSTICE DELAYED IS JUSTICE DENIED
In April 1963, authorities in Birmingham, Alabama arrested Dr. Martin Luther King for leading nonviolent civil rights protests that violated a court-ordered injunction. After his arrest, a multidenominational group of white religious leaders published a “A Call for Unity” that opposed King and his tactics. While acknowledging racial inequalities, they counseled patience, negotiations and pursuit of grievances through the courts.

In response, King penned a long “Letter from the Birmingham Jail” articulating his disappointment in their movement’s liberal supporters, the need to make racial injustice more visible and the universality of human suffering. It is a remarkable document. In it, he notes that the word “wait” almost always means “never” and quotes Chief Justice Earl Warren who famously observed “Justice delayed is justice denied.”
The following passage from King’s letter is particularly powerful.
History is the long and tragic story of the fact that privileged groups seldom give up their privileges voluntarily. Individuals may see the moral light and voluntarily give up their unjust posture; but, as Reinhold Niebuhr has reminded us, groups are more immoral than individuals.
Organizations pursue their interests with buzz-saw intensity. Such is the case with EHR companies. Their predatory business practices, while detrimental to healthcare delivery, have made them wealthy and powerful. They are loath to give up their privileges.
This is a watershed moment for healthcare. Liberated data saves lives. Maintaining the integrity of the proposed interoperability and data-blocking regulations is essential to advancing healthcare transformation.
This commentary begins with Fairview CEO James Hereford’s call for Epic to open its platform to innovative tech companies. He closed his remarks by suggesting a march on Epic’s headquarters by health system leaders could advance the cause.
“There is an opportunity for us to go to Epic and say, ‘Look, you have to open up this platform.’ It’s for our benefit in terms of having an innovative platform where all these bright, amazing entrepreneurs can actually have access to what is essentially 80 percent of the U.S. population that is cared for within an Epic environment. I would love for us to get together to see how we march on Madison.”
As Hereford’s insightful comments indicate, America has the capacity to make healthcare kinder, smarter and more affordable. ONC and CMS are doing their part to liberate healthcare data. They need the support of healthcare revolutionaries everywhere to make their proposed regulations the law of the land.
SOURCES
- https://www.bizjournals.com/twincities/news/2018/01/16/fairview-ceo-says-epic-an-impediment-to.html
- https://www.hitechanswers.net/ehr-adoption-2/meaningful-use/
- https://khn.org/news/death-by-a-thousand-clicks
- https://ehrintelligence.com/news/cerner-epic-systems-account-for-51.5-acute-care-hospital-market
- https://www.ncbi.nlm.nih.gov/pubmed/23860193/
- https://www.nytimes.com/2019/02/11/upshot/hospital-mergers-hurt-health-care-quality.html
- https://www.nytimes.com/2018/12/20/business/epic-systems-campus-verona-wisconsin.html
- https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers
- http://wtnnews.com/articles/212/
- https://www.beckershospitalreview.com/healthcare-information-technology/epic-founder-judy-faulkner-comes-in-3rd-on-forbes-richestwomen-list.html